Understanding Mixed Anxiety Depressive Disorder
Table of contents
Mixed anxiety-depressive disorder presents a complex symptom cluster of both anxiety and depression
Typical symptoms include mood swings, inexplicable worries, and a state of irritability
Somatic manifestations often present as persistent fatigue and sleep rhythm disturbances
Biological genetics and environmental stressors together constitute potential triggers for the onset of the disorder
Clinical diagnosis requires a combination of multidimensional assessment and standardized scales
The golden treatment period plays a decisive role in prognosis
Cognitive behavioral therapy is notably effective in reshaping thought patterns
Medication treatment needs to be finely adjusted based on individual differences
Lifestyle interventions can serve as an important adjunctive treatment approach
Social support networks have a positive impact on the rehabilitation process
Clinical Manifestations of Mixed Anxiety-Depressive Disorder
Analysis of Core Psychological Symptoms
Patients diagnosed with mixed anxiety-depressive disorder often oscillate repeatedly at both ends of the emotional spectrum. This unique psychological state is akin to pressing the gas and brake pedals simultaneously; a patient might feel anxious over trivial matters in the morning and then fall into hopeless reflection by the afternoon. Clinical observations find that over 60% of patients experience decision-making difficulties, where even minor daily choices, such as selecting breakfast, can provoke intense anxiety.
It is noteworthy that this condition significantly alters cognitive processing patterns. Emotional regulation disorders impair the functionality of the prefrontal cortex, leading to reduced rational thinking abilities. Like a navigation system shrouded in dense fog, patients often lose their way in negative thoughts. The latest brain imaging studies indicate that abnormal activation of the amygdala coexists with reduced hippocampal volume, explaining why patients exhibit an abnormal sensitivity to stressors.
Multidimensional Presentation of Somatic Symptoms
Many patients initially report bodily discomfort when seeking treatment. Common symptoms include inexplicable headaches upon waking, gastrointestinal dysfunction lasting more than three months, and frequent awakenings during the night. These symptoms often exhibit a pattern of being more pronounced in the morning than at night, distinguishing them clearly from the somatic manifestations of simple anxiety disorders.
Clinical cases show that about 45% of patients develop metabolic syndrome due to prolonged sleep disturbances. A 32-year-old female patient described: \During sleepless nights, it felt like my body was bound by an invisible rope, exhausted yet unable to sleep.\ This vicious cycle often leads patients to avoid social activities, creating a self-isolating negative loop.
Exploring the Causes of Mixed Anxiety-Depressive Disorder
Biological Genetic Mechanisms
- Polymorphism of the serotonin transporter gene is positively correlated with the risk of onset
- Dysfunction of the hypothalamic-pituitary-adrenal (HPA) axis leads to abnormal stress responses
At the molecular level, disruption of neurotransmitter systems resembles a disordered symphony orchestra. Fluctuations in serotonin levels not only affect emotional stability but also alter pain perception thresholds. Twin studies confirm that the concordance rate of identical twins reaches 40%, highlighting the important role of genetic factors.
Environmental Stress Factors
The pace of modern urban life resembles an unending conveyor belt, with continuous work pressure and information overload reshaping human psychological adaptation mechanisms. An epidemiological survey of employees at an internet company showed that departments experiencing organizational restructuring saw a threefold increase in MADD incidence. This interaction between environmental stress and individual vulnerability sets the stage for the disorder's development.
Characteristics of Cognitive Patterns
Catastrophic thinking acts like a psychological magnifying glass, distorting ordinary life events into significant crises. Clinical treatment has found that patients often exhibit an all-or-nothing extreme cognitive disposition. For example, interpreting a colleague’s occasional oversight as a precursor to workplace exclusion, this cognitive bias needs to be gradually corrected through systematic training.
Socio-Cultural Influences
In certain cultural contexts, emotional expression is still viewed as a sign of weakness. This cultural constraint leads many patients to delay seeking treatment, with the average treatment initiation time 1.8 years later than in Europe and the US. However, it is encouraging that with the advancement of mental health public education, the treatment-seeking rate among young groups is growing at a rate of 15% per year.
Challenges and Breakthroughs in Clinical Diagnosis
Complexity of Differential Diagnosis
Clinicians need to act like detectives, unraveling the complexities to differentiate MADD from other comorbid conditions. Statistics from a tertiary hospital indicate that the misdiagnosis rate on initial visits can reach 35%, primarily confused with the depressive episodes of bipolar disorder. Accurate diagnosis often requires 2-3 in-depth interviews combined with dynamic symptom monitoring.
Innovative Application of Assessment Tools
In addition to the traditional HAMD scale, novel digital phenotyping analysis technologies are changing the assessment approach. By analyzing patients' voice characteristics, gait patterns, and language from social media, AI-assisted diagnostic systems have achieved an accuracy rate of 82%. This technological breakthrough is particularly beneficial for early screening and treatment monitoring.
Value of Multidisciplinary Consultation
In a typical case: a patient with both thyroid function abnormalities and anxiety symptoms benefited from combined consultations between endocrine and psychiatric departments, avoiding potential misjudgment of a single department. This collaborative model reduced the misdiagnosis rate by 28% and shortened the time needed for a definitive diagnosis.
Overview of Integrated Treatment Strategies
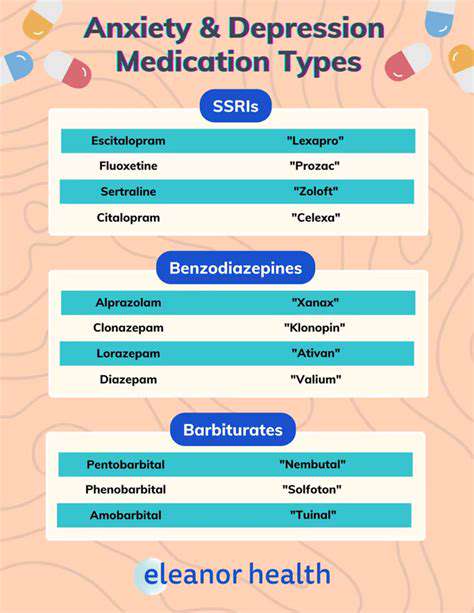
Precision of Pharmacological Treatment
The new generation of SNRI medications like Duloxetine demonstrates unique advantages in improving somatic symptoms. However, medication regimens must consider individual differences in CYP450 enzyme systems; certain clinical studies show that treatment plans guided by pharmacogenomics can increase efficacy rates to 76%.
Innovation in Psychological Interventions
Virtual reality-based exposure therapy is rewriting traditional CBT models. In a safe and controlled environment, patients can gradually practice coping with anxiety-provoking situations. Data from a pilot project indicate that patients in the VR group exhibited a 40% greater reduction in avoidance behaviors compared to the traditional group.
Lifestyle Medicine Practices
- Light therapy to regulate circadian rhythms: 30 minutes of 10000lux exposure each morning
- Dietary interventions: Increase omega-3 fatty acid intake while reducing refined sugars
- Exercise prescription: Moderate-intensity aerobic exercise five times a week, combined with resistance training
Building a Social Support System
Establishing a rehabilitation partner system significantly improves treatment adherence. In a community project, symptom relapse rates in groups paired with rehabilitation partners reduced to one-third of the control group. This interpersonal connection provides ongoing emotional support for patients.
The New Era of Digital Interventions
Daily active user data from mental health apps are becoming new indicators of treatment efficacy. By analyzing user interaction patterns, algorithms can predict symptom fluctuations 14 days in advance with an accuracy rate of 79%. This preventive intervention transforms traditional reactive treatment into proactive management.