Understanding IBS Related to Anxiety: Management Strategies
What's particularly cruel is how anxiety creates a vicious cycle. The more you worry about potential digestive disasters, the more likely they are to happen. It's like your brain keeps hitting the panic button, and your gut keeps answering the call. Before you know it, you're stuck in a loop where fear fuels symptoms, and symptoms fuel more fear.
IBS as a Trigger for Anxiety
Now flip the script: Imagine never knowing when your stomach might rebel. The constant uncertainty of IBS can turn everyday activities into potential minefields. Will there be a bathroom nearby? What if I have an attack during my meeting? This relentless unpredictability plants seeds of anxiety that can grow into full-blown worry trees.
The physical discomfort alone is enough to make anyone tense. But add in the social embarrassment and lifestyle limitations, and it's no wonder many IBS sufferers develop anxiety. It's not just about the pain - it's about how the condition chips away at your confidence and sense of control.
The Role of Gut Bacteria
Recent discoveries about our gut microbiome have added another fascinating layer to this story. 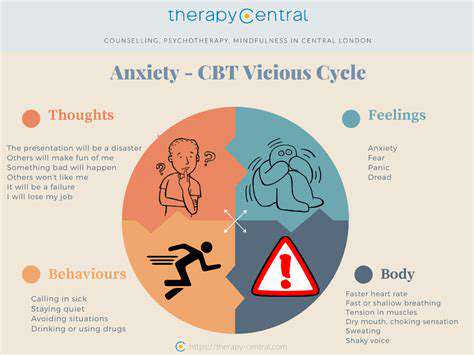 Turns out, the trillions of bacteria living in our digestive tract might be pulling more strings than we realized. When these microbial communities get out of balance, they can send chemical messages that affect everything from our mood to our bowel movements. Some researchers now believe that fixing gut bacteria might be key to treating both IBS and anxiety simultaneously.
Turns out, the trillions of bacteria living in our digestive tract might be pulling more strings than we realized. When these microbial communities get out of balance, they can send chemical messages that affect everything from our mood to our bowel movements. Some researchers now believe that fixing gut bacteria might be key to treating both IBS and anxiety simultaneously.
Treatment Strategies
Breaking the IBS-anxiety cycle requires a multi-pronged attack. Cognitive behavioral therapy has shown particular promise because it tackles the thought patterns that fuel both conditions. Meanwhile, dietary changes can calm the physical symptoms that trigger anxiety. The magic happens when we address both mind and gut together - like fixing both ends of a seesaw to achieve balance.
Coping Mechanisms and Support
Building a toolkit of relaxation techniques can make all the difference. Simple practices like focused breathing or progressive muscle relaxation act like circuit breakers for the anxiety-IBS feedback loop. Perhaps most importantly, finding community support reminds sufferers they're not alone in this battle. Whether through formal groups or trusted friends, sharing the struggle cuts the burden in half.
Lifestyle Modifications and Dietary Changes
Dietary Adjustments for IBS and Anxiety
What we eat directly impacts both our gut and mental health, making dietary changes a powerful weapon against IBS-anxiety. The key lies in personalization - there's no one-size-fits-all solution. Some find relief by eliminating trigger foods like garlic or beans, while others benefit from adding gut-friendly options like fermented foods. Keeping a detailed food-mood-symptom journal often reveals surprising connections between meals and symptoms.
Timing matters as much as content. Eating smaller, regular meals prevents the digestive system from getting overwhelmed. Staying hydrated is equally crucial - dehydration can mimic and worsen IBS symptoms. Working with a nutritionist who understands the gut-brain connection can help create a tailored plan that addresses both physical and emotional needs.
Stress Management Techniques for IBS-Related Anxiety
Chronic stress acts like fertilizer for both IBS and anxiety. Incorporating daily stress-busters can significantly dial down symptoms. Mindfulness practices teach us to observe discomfort without panicking, breaking the fear-pain cycle. Regular movement - whether yoga, walking, or dancing - releases tension and mood-boosting chemicals that benefit both mind and gut.
Sleep quality dramatically affects digestive health and emotional resilience. Creating a calming bedtime routine signals the body it's safe to rest. This might include gentle stretching, herbal tea, or journaling to empty worries from the mind. Protecting sleep is protecting your gut.
Lifestyle Changes and IBS Symptom Control
Beyond diet and stress relief, simple lifestyle tweaks can yield big results. Establishing routines provides predictability that anxious guts crave. Social connections buffer against stress - even when IBS makes going out challenging. The most effective approach combines physical care with emotional support, recognizing that IBS and anxiety feed on isolation.
Professional guidance can help tailor these strategies to individual needs. A gastroenterologist addresses the physical aspects, while a therapist helps untangle the emotional components. Together, they form a dream team for reclaiming quality of life from these intertwined conditions.
Seeking Professional Help
Understanding the Connection
The IBS-anxiety link resembles a tangled knot - pulling one string tightens the other. Recognizing this interconnection is the first step toward effective treatment. Symptoms often fluctuate together, creating patterns that trained professionals can help decode. Specialists now understand that treating just one condition often leads to incomplete results - the most successful approaches address both simultaneously.
Identifying Anxiety-Related IBS Symptoms
Spotting anxiety's fingerprint on IBS symptoms requires detective work. Notice when symptoms spike - during stressful events? After anxious thoughts? Tracking these patterns reveals connections that guide treatment. Many patients discover their gut reacts to emotional triggers before their conscious mind registers the stress, making the body an early warning system.
The Role of Stress in IBS
Stress doesn't just live in our minds - it manifests physically through gut reactions. The digestive tract contains as many neurons as the spinal cord, essentially forming a second brain. When stressed, this enteric nervous system goes haywire, causing the spasms and sensitivity characteristic of IBS. Managing stress effectively often brings more relief than dietary changes alone.
Psychological Factors and IBS
The mind-gut connection explains why psychological therapies help IBS. Techniques that reduce catastrophic thinking (This pain means something terrible) directly calm digestive distress. Many IBS sufferers unknowingly maintain symptoms through fear-based behaviors, like overly restricting foods or avoiding activities. Therapy helps rebuild confidence and flexibility.
Dietary Strategies for Anxiety-Related IBS
Nutritional approaches must account for both physical sensitivities and emotional needs. Restrictive diets can backfire by increasing food anxiety. The most sustainable plans gradually reintroduce foods while building coping skills. Probiotic-rich foods may pull double duty by supporting gut health and mood regulation through the microbiome.
Lifestyle Modifications for Symptom Relief
Small, consistent changes create ripple effects. Regular mealtimes regulate digestion and reduce decision fatigue. Gentle movement maintains gut motility without triggering stress responses. Perhaps most importantly, cultivating self-compassion softens the frustration of chronic symptoms, making the journey more manageable.
Seeking Professional Support
Specialized help can break logjams in the IBS-anxiety cycle. Gastroenterologists rule out other conditions and suggest gut-directed treatments. Mental health professionals provide tools to short-circuit the stress-digestion feedback loop. The most effective care happens when these specialists collaborate, creating a unified treatment plan that addresses the whole person.