The Connection Between OCD and Insomnia: Exploring Relationships
Understanding Insomnia
Insomnia, characterized by persistent difficulty falling asleep, staying asleep, or experiencing restful sleep, affects countless individuals globally. While often dismissed as mere restlessness, it frequently signals deeper physiological or psychological concerns. Identifying insomnia's underlying triggers proves essential for meaningful recovery, whether they stem from medical conditions, emotional distress, or environmental factors.
This sleep disorder doesn't merely cause fatigue - it reshapes cognitive function and emotional resilience. The cumulative effect of poor sleep manifests in reduced productivity, strained relationships, and diminished life satisfaction, making early intervention critical.
How Sleep Loss Alters Brain Chemistry
When the brain misses its necessary restorative cycles, fundamental changes occur at the neurological level. Neurotransmitter imbalances emerge, particularly in serotonin and dopamine systems, directly influencing thought patterns and behavioral responses. Sleep-deprived individuals often experience heightened amygdala activity, creating exaggerated fear responses and reduced prefrontal cortex functionality - the exact neural conditions that foster obsessive thinking.
These biochemical shifts don't simply cause tiredness; they rewire decision-making processes and emotional regulation capacities. The resulting mental state becomes fertile ground for compulsive behaviors as the exhausted brain seeks predictable patterns to compensate for impaired judgment.
Anxiety's Amplifying Effect on OCD Patterns
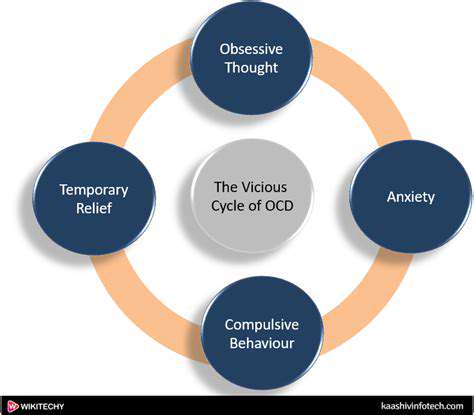
Obsessive-Compulsive Disorder manifests through intrusive mental narratives and ritualized physical responses, both serving as maladaptive coping mechanisms. The disorder thrives in environments of psychological uncertainty, where compulsive behaviors temporarily alleviate distress before reinforcing the anxiety cycle. What many overlook is how chronic sleep deprivation systematically erodes the mental resources needed to resist these patterns.
Stress hormones like cortisol remain elevated in sleep-deprived individuals, directly intensifying OCD symptom severity. This creates a self-perpetuating loop where obsessive thoughts disrupt sleep, and sleep loss exacerbates obsessive thinking - a dynamic requiring specialized therapeutic interruption.
The Bidirectional Nature of Sleep and Anxiety
Sleep specialists increasingly recognize the reciprocal relationship between rest quality and emotional stability. Racing thoughts prevent sleep onset, while fatigue heightens sensitivity to stressors the following day. This creates a self-sustaining feedback loop that often requires simultaneous intervention - addressing either component in isolation yields limited results. The neurological basis for this connection lies in how sleep regulates emotional memory processing.
During REM cycles, the brain naturally processes and diffuses emotional charges from daily experiences. Without this critical phase, negative emotions accumulate, lowering the threshold for anxiety responses. Modern therapeutic approaches now emphasize sleep restoration as foundational to anxiety treatment.
How Sleeplessness Fuels Obsessive Patterns
Emerging research reveals disturbing parallels between sleep-deprived cognition and OCD symptom profiles. Sleep fragmentation specifically increases thought fixation tendencies, while fatigue impairs the cognitive flexibility needed to dismiss intrusive ideas. Clinicians report that patients with untreated insomnia frequently develop compulsive checking behaviors related to sleep preparation routines.
The prefrontal cortex's diminished capacity for error detection during sleep loss creates ideal conditions for compulsive rituals to take root. Furthermore, the hyperarousal state characteristic of chronic insomnia mirrors the physiological aspects of OCD, suggesting shared neurological pathways worth exploring in treatment.
Integrated Treatment Methodologies
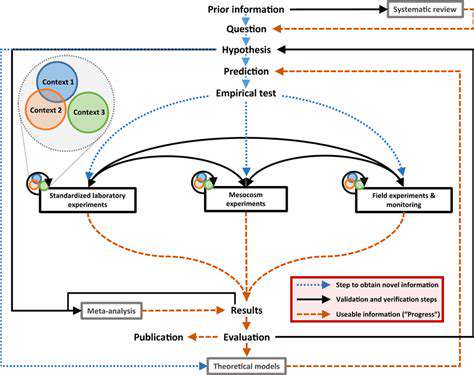
Progressive treatment plans now combine sleep hygiene protocols with exposure therapy techniques. Stimulus control therapy for insomnia pairs remarkably well with response prevention for OCD, as both require systematic habituation to discomfort. Light therapy for circadian rhythm adjustment often complements these approaches, particularly for patients with evening compulsions that delay sleep onset.
Nutritional psychiatry interventions have shown promise in concurrent treatment, with specific amino acid protocols supporting both serotonin production and melatonin regulation. This biological component, combined with cognitive restructuring techniques, creates a comprehensive approach to breaking the insomnia-OCD cycle.
Every memorable event begins with a well-defined purpose. Unlike fleeting thoughts, this represents a vivid mental blueprint of your desired outcome. The most successful celebrations blend practical elements with emotional resonance, creating experiences that linger in guests' memories. This approach requires identifying what genuinely matters to you and ensuring every decision reflects those priorities.