Coping with Pregnancy Related Anxiety: Tips and Support
Practical solution: Create three financial plans—ideal, manageable, and survival-mode. Having contingency blueprints reduces the what if spiral. As one financial planner told her pregnant clients: Worry is interest paid on debt not yet owed.
Health Concerns and Worries About the Baby
Modern medicine gives us fetal heartbeat apps—and with them, 24/7 opportunities to panic over slight variations. The paradox of information: More data means more variables to obsess over. One study found 68% of pregnant women Googled symptoms daily, with 42% experiencing increased anxiety afterward.
Midwives observe a telling pattern: mothers who felt their baby kick too much and too little often sat in adjacent waiting rooms. This highlights pregnancy anxiety’s cruel duality—the same symptom can trigger opposite fears.
Relationship and Family Dynamics
A couple’s hidden curriculum emerges during pregnancy—unspoken expectations about who handles midnight feedings or whether grandparents get naming rights. These unvoiced assumptions become landmines when stress runs high. Therapists report a surge in sessions around week 28, when reality sets in.
Pro tip: Role-play tough conversations beforehand. Practice saying, When you said ___, I felt ___ with your partner. It feels silly until it saves your sanity during a 3 AM argument about pacifier brands.
Lifestyle Adjustments and Changes
That first time you decline sushi or skip spin class makes it real: your body isn’t fully yours anymore. The loss of autonomy hits harder than expected. One CEO confessed crying in her car after realizing she’d miss her annual backpacking trip—not because of the trip itself, but what its cancellation symbolized.
Social Expectations and Pressures
Instagram vs. reality: While influencers post glowing bump photos, actual pregnant women vomit in parking lots. The pressure to perform happy pregnancy while feeling miserable creates cognitive dissonance. Doula communities now host real talk sessions where women share unfiltered experiences—stretch marks, hemorrhoids, and all.
Past Experiences and Trauma
For women with pregnancy loss history, each milestone—12-week scan, quickening—brings relief and fresh terror. The mind becomes a pendulum swinging between everything’s fine and disaster is imminent. Specialized therapists use techniques like EMDR to reprocess traumatic memories, helping patients stay present.
Connecting with Your Support Network
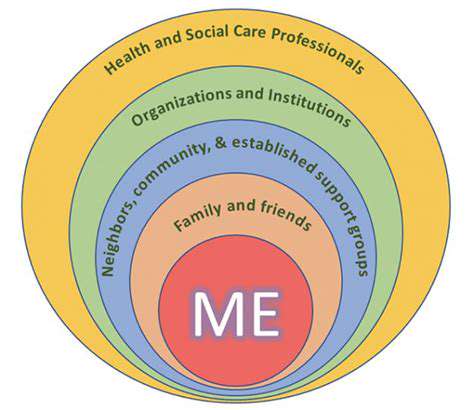
Understanding the Importance of Support
Anthropologists note that human pregnancy evolved to be a communal experience—yet modern life isolates expectant parents. This disconnect explains why pregnancy classes reduce anxiety by 37%: they recreate the ancestral village. Your great-grandmother had aunts and neighbors sharing wisdom; you have Facebook groups and Reddit threads. Both serve the same primal need.
Identifying Your Support System
Think beyond the obvious. That barista who remembers your decaf order? Potential support. The pharmacist who explains medications without rushing you? Support. Build a constellation of helpers—not everyone needs to be a supernova. One mother’s most comforting third-trimester texts came from her dry cleaner, a fellow twin parent.
Building a Supportive Environment
Create a pregnancy password with loved ones. For example: When I say ‘peanut butter,’ it means I need help but can’t articulate why. Pre-established codes bypass the shame spiral of I shouldn’t need this much help. One couple used avocado as their distress signal—it made requests feel lighter.
Seeking Support When Needed
Note this paradox: the times you least want to reach out are when you most need to. Pregnancy hormones can convince you that burdening others is unforgivable. Combat this by pre-scheduling check-ins. Put Text Maya on your calendar every Tuesday—no waiting until you deserve support.
Maintaining Healthy Boundaries
Your mother-in-law’s daily bump inspection requests? The coworker who trauma-dumps about her niece’s stillbirth? Pregnancy turns you into an emotional lighthouse—some will try to dock their issues at your shore. Practice: I’m focusing on my mental health right now with a subject-changing smile.
Navigating Conflicts Within Your Network
Hormonal changes can make conflicts feel apocalyptic. Before reacting to that careless comment, ask: Will this matter in six months? One couple kept a fight jar—each put in $20 when bickering over nursery colors. The money funded their first date night postpartum, transforming arguments into future connection.
Expanding Your Support Network
Seek horizontal support—peers at the same pregnancy stage. There’s unique comfort in complaining about hemorrhoids with someone who also can’t see their feet. Apps like Peanut function like Tinder for mom-friends, matching by due date and parenting philosophy.
Designing functional spaces parallels pregnancy preparation—both require adapting environments for new priorities. Just as kitchen work triangles optimize movement, arrange your home for pregnancy’s physical changes. Keep nausea crackers bedside, create a pregnancy station with vitamins and journals, and—critically—position charging cords within easy reach of nesting spots. These micro-adjustments prevent daily friction points that cumulatively drain emotional reserves.
Seeking Professional Help: When to Reach Out

Recognizing the Signs
When dread outweighs excitement more days than not, it’s time to intervene. Clinicians look for broken record thoughts—the same worry looping for over 72 hours. Physical red flags include scanxiety before appointments (racing heart, nausea beyond morning sickness) or obsessive behaviors like taking 10+ pregnancy tests weekly.
Understanding Your Needs
Perinatal mental health specialists categorize needs into tiers: Tier 1 (preventative): Normal worries needing coping tools. Tier 2 (reactive): Situational depression after a scary ultrasound. Tier 3 (clinical): Intrusive thoughts about harm coming to the baby. Knowing your tier guides treatment intensity.
Finding the Right Professional
Seek providers certified in perinatal mental health (PMH-C). They understand pregnancy’s unique neurobiology—like how progesterone withdrawal mimics depression symptoms. Interview potential therapists: How would you handle my middle-of-the-night crisis texts? The right answer involves pre-established protocols, not just Call 911.
Exploring Treatment Options
Beyond talk therapy: Biofeedback trains you to control stress responses visible on screens. ART (Accelerated Resolution Therapy) reprograms traumatic memories in 1-5 sessions. Group therapy with other expectant parents normalizes struggles through shared vulnerability.
Taking the First Step
Booking that first appointment is hardest. Try the 5-minute rule: Tell yourself you’ll only make the call for five minutes. Hang up if it’s too much. Most find that once started, they continue. Another trick: Email therapists while in a waiting room—the distraction lowers the emotional barrier.
Building a Positive Mindset for a Healthy Pregnancy
Understanding the Impact of Stress
Chronic stress floods the womb with cortisol—the baby’s first environment becomes a stress soup. But here’s hope: Research shows maternal resilience behaviors (like reframing negative thoughts) actually alter fetal brain development positively. You’re not just managing stress—you’re programming your child’s future stress responses.
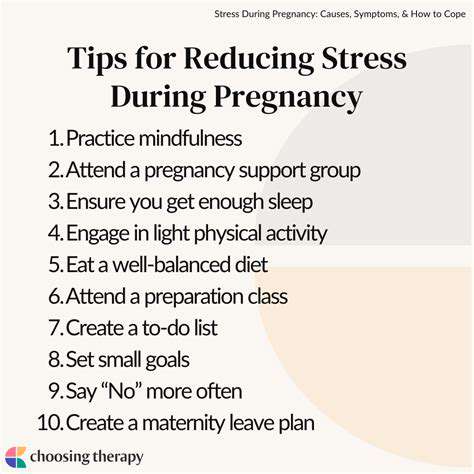
Cultivating Self-Care Practices
Forget spa days—real pregnancy self-care looks different. Radical rest means napping without guilt. Nutritional grace allows for salad one day, fries the next. One mom’s mantra: My job isn’t to be perfect—it’s to stay sane enough to make good decisions most of the time.
Nourishing Your Body and Mind
The gut-brain axis becomes crucial during pregnancy. Probiotic-rich foods (kimchi, kefir) may lower prenatal depression risks by 25%. Hydration isn’t just about water—electrolyte imbalances mimic anxiety symptoms. Carry salty snacks; low sodium triggers stress hormones.
Building a Supportive Network
Create a pregnancy council with specific roles: The Logical Friend (for when you’re spiraling), The Veteran Mom (been-there wisdom), The Cheerleader (celebrates every milestone). Delegate needs intentionally—don’t expect one person to be everything.
Managing Financial Worries
Financial therapists suggest reframing: Instead of We can’t afford this, try We’re choosing where to allocate resources. This subtle shift activates problem-solving instead of panic. Automate small savings transfers—watching the baby fund grow builds tangible security.
Seeking Professional Help When Needed
OBs now screen for mental health at every visit using simple scales. Scoring high isn’t failure—it’s accessing resources earlier. Think of it like gestational diabetes testing: identifying needs for specialized support.
Understanding and Accepting Changes
Try body neutrality if positivity feels forced. Instead of I love my stretch marks, try These marks represent my body’s incredible adaptability. Neutrality creates space for complex feelings without pressure to perform gratitude. Some days, that’s the healthiest mindset of all.