Signs of OCD: Identifying Symptoms Early
Taking your entertainment setup beyond the standard flat-screen TV involves more than just upgrading the resolution. Let's be honest - we've all seen those living rooms where the massive TV dominates the space like an unwelcome guest. The real magic happens when technology blends seamlessly with personal comfort and style. It's not about chasing specs; it's about crafting moments. Imagine dimmable lights that adjust with the movie's mood, seating that hugs you just right during long binge sessions, and sound that makes you feel explosions in your bones. That's the difference between watching and experiencing.
Beyond the Basics: Exploring Co-occurring Conditions
Understanding the Complexity of Co-occurring Conditions
Mental health rarely travels alone. Like uninvited plus-ones at a party, conditions often arrive in groups, each influencing the other in unpredictable ways. Take OCD - it rarely comes without its frequent companions, anxiety and depression. These aren't just additional checkboxes on a form; they change how symptoms present themselves. A patient's compulsive hand-washing might look textbook until you notice the depressive slump in their shoulders or the anxious tremor in their voice. Spotting these subtle interactions requires more than textbook knowledge - it demands human intuition and experience.
Diagnosis becomes a puzzle where pieces from different boxes get mixed together. That's why cookie-cutter treatments often fail. When conditions overlap, they create unique symptom cocktails that standard protocols can't address. This complexity explains why some patients feel stuck in treatment - their depression medication might be working while their OCD symptoms worsen, or vice versa. Only by mapping all the interconnected symptoms can clinicians chart an effective course forward.
The Impact on Treatment Approaches
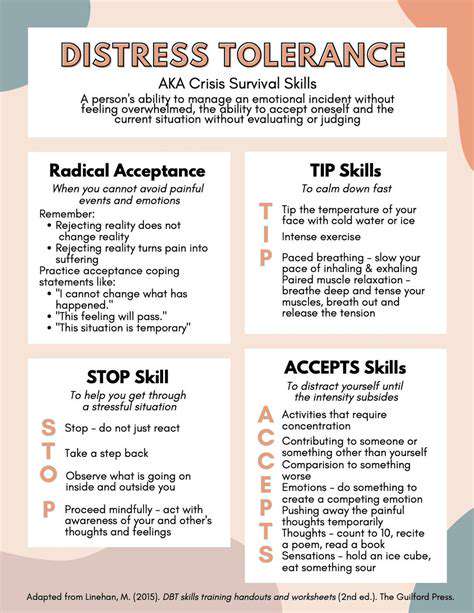
Standard treatment manuals gather dust when facing co-occurring conditions. Therapists often find themselves blending techniques like master chefs - a dash of CBT for OCD here, a sprinkle of DBT for emotional regulation there. Medication decisions become delicate balancing acts. An SSRI might help OCD but exacerbate anxiety symptoms in some patients. The art lies in finding the right combination that addresses all conditions without creating new problems.
Timing matters too. Treating the most debilitating condition first often creates a foundation for addressing others. But sometimes, small improvements in one area can unexpectedly relieve symptoms elsewhere. This unpredictable interplay demands flexible treatment plans that evolve as the patient progresses, not rigid protocols set in stone.
The Role of Professional Assessment
Ever tried solving a jigsaw puzzle blindfolded? That's what diagnosing co-occurring conditions without thorough assessment feels like. Good clinicians don't just check symptoms; they become detectives piecing together life histories. That irrational fear might trace back to childhood trauma. The sleep disturbances could stem from undiagnosed ADHD. Quality assessment digs deeper than surface symptoms to uncover root causes and connections.
The best assessments feel like conversations, not interrogations. They create space for patients to share what they might not even realize is relevant - that family history of alcoholism, the job stress they've normalized, or how their symptoms change with seasons. These details often hold the keys to accurate diagnosis and effective treatment.
Strategies for Effective Management
Managing multiple conditions isn't about fighting separate battles - it's about building an ecosystem of wellness. Think of it like tending a garden where different plants (conditions) need different care but share the same soil (the person). Mindfulness might water the anxiety plant while exercise strengthens the depression plant's roots. True progress happens when treatments work synergistically rather than in isolation.
Small daily practices often create ripple effects. A morning gratitude journal might unexpectedly reduce compulsive thoughts. Regular sleep patterns could ease both anxiety and depression symptoms. These lifestyle adjustments become the foundation that makes other treatments more effective.
The Importance of Support Systems
Healing happens in connection, not isolation. The right support system acts like scaffolding for someone rebuilding their mental health. But not all support helps equally. Well-meaning family members might accidentally enable compulsions. Friends might dismiss symptoms with just relax advice. The most effective supporters learn to provide the right balance of compassion and challenge.
Support groups offer something unique - the powerful realization of I'm not alone. There's magic in hearing someone else describe your exact struggle. These connections combat the isolation that often worsens mental health conditions. They also become laboratories for practicing new coping skills in safe environments before using them in daily life.