Anxiety with Psychotic Features: Symptoms and Coping Mechanisms
Defining Anxiety with Psychotic Features
Understanding the Core Concept
Anxiety with psychotic features represents a multifaceted mental health condition where individuals experience both intense anxiety and psychotic symptoms simultaneously. This dual presentation creates unique diagnostic challenges, as clinicians must untangle the overlapping manifestations of these distinct yet interconnected issues. The anxiety component typically involves persistent worry, irrational fears, and physical symptoms like rapid heartbeat, while psychotic elements may include auditory hallucinations, paranoid delusions, or fragmented thought processes.
Recent clinical observations suggest the relationship between anxiety and psychosis operates cyclically - each potentially amplifying the other. This bidirectional influence underscores the importance of comprehensive evaluation methods that consider symptom onset patterns, environmental triggers, and the patient's full psychiatric history. Treatment specialists emphasize that overlooking this complexity can lead to inadequate care approaches.
Differentiating Symptoms from Other Conditions
Accurate diagnosis requires meticulous differentiation from similar conditions like schizophrenia spectrum disorders or severe panic attacks with derealization. While schizophrenia typically presents with more persistent psychotic symptoms, anxiety-related psychosis often shows fluctuating intensity directly correlated with anxiety levels. Key distinguishing features include the episodic nature of symptoms and the presence of anxiety as the primary driver of psychotic experiences rather than independent psychotic illness.
Diagnostic protocols now incorporate advanced assessment tools including structured clinical interviews and longitudinal symptom tracking. These methods help identify subtle but crucial differences, such as how patients retain varying degrees of insight during psychotic episodes when anxiety constitutes the root cause. Such distinctions prove vital for determining appropriate pharmacological and therapeutic interventions.
Effective Management and Treatment Strategies
Contemporary treatment models advocate for integrated approaches combining carefully calibrated medication regimens with specialized psychotherapies. Pharmacological strategies often employ anxiolytics alongside low-dose antipsychotics, with close monitoring for medication interactions and side effect profiles. Emerging research highlights the particular effectiveness of clonazepam when combined with cognitive therapies for this dual diagnosis.
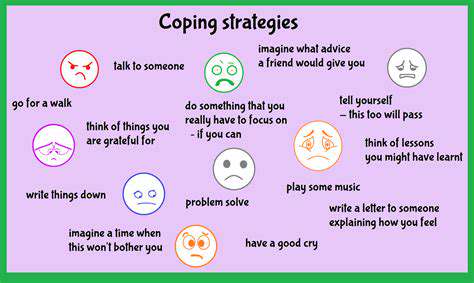
On the therapeutic front, modified CBT protocols address both symptom clusters simultaneously. These adapted approaches help patients identify anxiety triggers that precede psychotic symptoms while developing concrete coping strategies. Family psychoeducation programs have shown particular promise, equipping support networks to recognize early warning signs and implement de-escalation techniques effectively.
Coping Strategies and Treatment Approaches
Understanding Coping Mechanisms
Human stress responses manifest through diverse coping strategies that develop over a lifetime. These psychological tools range from highly adaptive to potentially harmful, with most individuals employing a mixture depending on circumstances. Contemporary psychology emphasizes the concept of coping flexibility - the ability to consciously select different strategies based on situational demands rather than relying on habitual responses.
Developing Healthy Coping Strategies
Building an effective coping repertoire requires deliberate practice and self-reflection. Evidence-based approaches recommend starting with small, manageable stressors to test and refine techniques. Progressive muscle relaxation, for instance, shows particular efficacy when practiced regularly before stressful situations arise. Behavioral activation - scheduling pleasant activities as buffers against stress - represents another research-backed method with cumulative benefits.
Seeking Professional Support
When self-directed coping efforts prove insufficient, professional guidance can provide transformative support. Modern therapeutic approaches move beyond generic advice to offer personalized strategy development. Specialized modalities like Acceptance and Commitment Therapy (ACT) help patients develop psychological flexibility - the ability to adapt coping methods to different emotional challenges while maintaining value-driven actions.
The Role of Mindfulness in Coping
Neuroscientific research has illuminated how mindfulness practices physically alter stress response pathways in the brain. Regular practitioners demonstrate measurable changes in amygdala reactivity and prefrontal cortex regulation. These biological changes correlate with improved emotional regulation capacities, making mindfulness particularly valuable for individuals managing co-occurring anxiety and psychotic symptoms.
Treatment Approaches for Emotional Well-being
The current therapeutic landscape offers numerous evidence-based options tailored to different needs. Schema Therapy, for example, proves particularly effective for individuals with longstanding maladaptive coping patterns. Newer approaches like Mentalization-Based Treatment show promise for those struggling with emotional regulation in interpersonal contexts.
The Importance of Lifestyle Factors
Emerging research continues to reveal the profound interconnection between physical health and emotional resilience. Gut microbiome health, for instance, demonstrates surprising correlations with stress response systems, suggesting dietary interventions may complement traditional coping strategies. Similarly, chronobiology research highlights how aligning activities with natural circadian rhythms can enhance coping capacity.
Building Support Systems
Social neuroscience confirms that quality relationships literally rewire our brains for better stress management. Purposeful relationship cultivation - focusing on depth rather than breadth of connections - appears most protective against stress-related health impacts. Community-based approaches that combine social support with skill-building show particular promise in clinical trials.
Promoting Wellbeing and Living a Full Life

Promoting Physical Health
Contemporary wellness models emphasize physical health as the foundation for comprehensive wellbeing. Innovative approaches now focus on movement quality rather than just quantity, with techniques like functional fitness gaining prominence. Nutritional psychiatry represents another growing field, investigating how specific dietary patterns influence mental health outcomes.
Cultivating Mental Resilience
Modern resilience training incorporates evidence-based techniques from positive psychology and neuroscience. Deliberate practice of cognitive reappraisal - reframing challenges as opportunities - shows measurable benefits in neuroimaging studies. Similarly, purpose cultivation exercises help individuals connect daily actions to larger meaning, buffering against stress.
Nurturing Social Connections
Quality relationships function as psychological safety nets during challenging times. Research confirms that even brief positive social interactions trigger oxytocin release, reducing physiological stress markers. Community-building initiatives that combine social connection with shared purpose demonstrate particularly strong wellbeing benefits across diverse populations.