Anxiety Induced IBS: Understanding the Connection

The Intertwined Worlds of the Gut and Brain
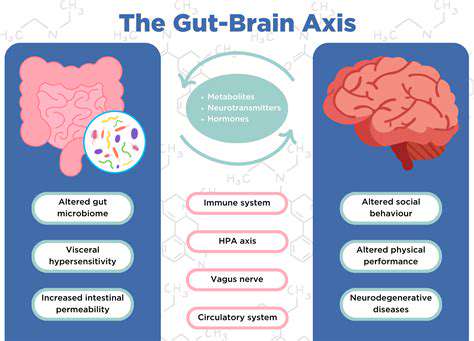
The human gut, often perceived as a simple digestive organ, is increasingly recognized as a crucial player in overall health, including mental well-being. This intricate connection, known as the mind-gut connection, highlights the dynamic interplay between the gut microbiome, the nervous system, and the brain. Understanding this complex relationship is critical for developing effective strategies to promote both physical and mental health.
The gut microbiome, a vast community of bacteria, fungi, and other microorganisms residing in the digestive tract, plays a pivotal role in this interaction. This community, often described as a hidden organ, produces neurochemicals that influence brain function, thereby affecting mood, behavior, and even cognitive abilities.
The Gut Microbiome's Influence on Mood
Emerging research strongly suggests that imbalances in the gut microbiome can contribute to mood disorders like depression and anxiety. These imbalances, often referred to as dysbiosis, can disrupt the delicate balance of neurochemicals in the brain, leading to emotional instability. Maintaining a healthy gut microbiome is therefore crucial for emotional well-being.
The gut microbiome produces neurotransmitters, such as serotonin and dopamine, which are vital for regulating mood. Imbalances in these neurotransmitters can manifest as mood swings, irritability, and increased susceptibility to stress.
The Role of the Nervous System
The enteric nervous system, often called the second brain, is a complex network of nerves embedded within the gut wall. This intricate system communicates constantly with the central nervous system, transmitting information that impacts mood, stress responses, and cognitive function. This bidirectional communication highlights the intricate link between the gut and the brain.
The vagus nerve, a crucial component of the enteric nervous system, plays a significant role in this communication pathway. It allows for the transmission of signals between the gut and the brain, influencing various physiological processes.
Dietary Impact on the Mind-Gut Connection
The foods we consume directly impact the composition and function of the gut microbiome. A diet rich in fiber, fruits, and vegetables promotes the growth of beneficial bacteria, while processed foods and excessive sugar intake can disrupt the delicate balance of this ecosystem. A balanced diet, rich in nutrients, is essential for maintaining a healthy gut microbiome and fostering a positive mind-gut connection.
Stress and the Gut-Brain Axis
Chronic stress has a profound impact on both the gut and the brain. Stress hormones released during stressful situations can disrupt the gut microbiome and influence the activity of the enteric nervous system, ultimately affecting mood and cognitive function.
Stress management techniques, such as meditation and mindfulness, can help regulate the stress response and promote a healthier mind-gut connection.
The Impact of Gut Health on Cognitive Function
Emerging research suggests that the gut microbiome might even play a role in cognitive functions like memory and learning. The presence of specific bacteria in the gut may influence the production of neurochemicals that support cognitive processes. A healthy gut environment may therefore contribute to optimal cognitive performance.
The Future of Mind-Gut Research
The mind-gut connection is a rapidly evolving area of research, promising exciting possibilities for understanding and treating a wide range of health conditions. Further investigation into the intricate mechanisms underlying this connection is crucial for developing targeted interventions that promote both physical and mental well-being. Ongoing research endeavors aim to unravel the complex interactions between the gut, the nervous system, and the brain and their influence on various health conditions.
Sudden vomiting, a distressing experience for anyone, often stems from a variety of underlying causes, some benign and easily resolved, while others necessitate prompt medical attention. Viral gastroenteritis, frequently referred to as the stomach flu, stands as a prevalent trigger, causing inflammation of the digestive tract and leading to nausea, vomiting, diarrhea, and abdominal cramps, typically resolving within a few days with supportive care, including hydration and rest. Food poisoning, another frequent culprit, occurs when consuming contaminated food containing bacteria, viruses, or toxins, resulting in rapid onset vomiting, often accompanied by fever, chills, and other gastrointestinal distress, requiring careful monitoring and, in some cases, medical intervention to prevent dehydration and complications.
Managing Anxiety and IBS: A Holistic Approach

Understanding the Connection
Anxiety and Irritable Bowel Syndrome (IBS) are often intertwined, creating a vicious cycle where one condition exacerbates the other. Anxiety can trigger or worsen IBS symptoms, such as abdominal cramping, bloating, and diarrhea. Conversely, the discomfort and unpredictability of IBS can lead to increased anxiety and stress, further fueling the cycle. Understanding this connection is crucial for effective management and treatment.
Research suggests a strong link between the gut-brain axis, which refers to the complex communication network between the digestive system and the brain. This bidirectional communication pathway plays a critical role in influencing mood and behavior, emphasizing the significant impact that gut health has on mental well-being, and vice versa.
Dietary Strategies for Relief
A balanced and mindful approach to diet is often beneficial for both anxiety and IBS. Identifying and eliminating trigger foods, such as processed foods, caffeine, and certain dairy products, can significantly reduce IBS symptoms. Focusing on a diet rich in fiber, fruits, and vegetables is essential for promoting digestive health and regularity.
Mindfulness and Relaxation Techniques
Mindfulness practices, such as meditation and deep breathing exercises, can help manage anxiety and reduce IBS symptoms. These techniques promote relaxation and a sense of calm, potentially decreasing the physiological responses that contribute to IBS discomfort. By incorporating mindfulness into daily routines, individuals can develop coping mechanisms for managing stress and anxiety.
Physical Activity and Stress Reduction
Regular physical activity can significantly reduce stress and anxiety levels, which can, in turn, improve IBS symptoms. Exercise releases endorphins, which have mood-boosting effects, and helps regulate the body's stress response, contributing to a more balanced physiological state. Finding activities you enjoy, such as walking, swimming, or yoga, can make incorporating exercise into your routine more sustainable and enjoyable.
Seeking Professional Guidance
When anxiety and IBS symptoms significantly impact daily life, seeking professional guidance is essential. A gastroenterologist can diagnose IBS and rule out other potential medical conditions. A therapist or counselor can provide support and strategies for managing anxiety and stress. Collaboration between medical and mental health professionals is often vital for comprehensive and effective treatment.
Lifestyle Adjustments for Improved Well-being
Beyond diet and physical activity, several lifestyle adjustments can contribute to overall well-being and help manage both anxiety and IBS. These include getting adequate sleep, establishing a regular sleep schedule, and limiting alcohol and nicotine consumption. Prioritizing sufficient sleep is crucial, as sleep deprivation can exacerbate both anxiety and digestive issues. Creating a supportive social network and engaging in enjoyable hobbies can also enhance emotional well-being and reduce stress.